Report Finds Optometry Eye Care Interventions Could Avoid up to 1.9 Million Appointments in Pressured NHS Services Annually
29 November 2024
A first-of-its-kind analysis, conducted by PA Consulting and commissioned by Primary Eyecare Services, the Association of Optometrists (AOP), Fight for Sight, and Roche, reveals the often-overlooked clinical and socio-economic benefits of primary eye care.
The report emphasises how this sector can significantly improve public health outcomes in the UK, while saving the NHS approximately £98 million each year.
Titled ‘Key Interventions to Transform Eye Care and Eye Health’, the report sheds light on the potential of high-street optometry practices to transform the delivery of eye care.
This comprehensive report is a timely intervention given the cost pressures ICBs continue to face and the extreme financial scrutiny of all services. It outlines strategic interventions designed to enhance eye care services, improve patient outcomes, and optimise the use of resources within the NHS. The report aligns with the findings of the Darzi Report and supports the government’s three key pillars: transitioning from hospital to community care, shifting from sickness to prevention, and moving from analogue to digital healthcare.
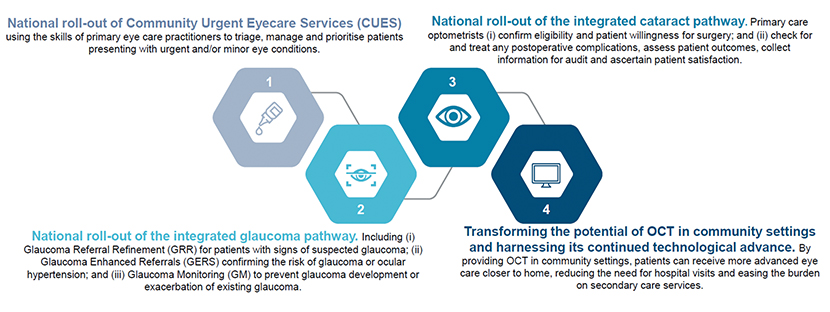
The key interventions beyond GOS are as follows:
Key Findings From the Report
Economic and Operational Benefits
The report highlights that the national roll-out of the four proposed interventions could result in approximately £98 million in net direct cost savings to the NHS annually and more importantly reduce NHS appointments by 1.9 million, including reductions in Hospital Eye Services (HES), A&E, and GP appointments. (Recognising that some of these impacts are already being realised where the interventions are already commissioned and being delivered locally.)
Enhanced Patient Access and Outcomes
The interventions are expected to provide faster, more convenient access to integrated eye care and eye health services for patients, maximising the use of technology and data to improve outcomes.
Support for National and Local Implementation
The report emphasises the need for strong national support and local action to realise the benefits of these interventions, including leadership from government and NHS bodies, and collaboration with professional associations and patient groups.
Addressing Workforce Challenges
The report identifies significant workforce challenges in hospital eye services, with only 24% of eye units believing they have enough consultants to meet current demand. The proposed interventions aim to relieve pressure on HES and allow clinicians to focus on more complex cases.
PA Consulting’s analysis used a logic model to quantify service shifts, estimating appointment reductions and translating these into cost savings by comparing community and hospital service costs. After deducting national rollout costs, the net financial benefit was calculated. Beyond financial savings, these interventions promise qualitative improvements, such as enhanced patient convenience, reduced anxiety from quicker care, and improved staff satisfaction through reduced hospital strain and more clinical work in community settings.
Dharmesh Patel, Chief Executive of Primary Eyecare Services said: “This report emphasises the critical need to expand eye care services within primary care optometry settings to alleviate the burden on GPs, A&E and hospital ophthalmology, enhancing patient care and supporting NHS sustainability.”
With long waiting times continuing to pose challenges for patients and the NHS, this report highlights interventions based on existing innovative delivery models utilising primary and community optometry practices. Along with partners, we stand ready to scale up delivery of eye care in the community at a local, regional and national level at pace.”
Further information can be found on the AOP website here.
Note: This report is by PA Consulting. The Association of Optometrists, Fight for Sight, Primary Eyecare Services and Roche Products Ltd have provided financial support for this activity and have had editorial input and reviewed all associated output.